Tuberculosis (TB)
Subscribers of "Current Affairs" course can Download Daily Current Affairs in PDF/DOC
Subscribe to Never Miss an Important Update! Assured Discounts on New Products!
Must Join PMF IAS Telegram Channel & PMF IAS History Telegram Channel
- Context (TH | TH | TH | TH): On March 24, World TB Day was celebrated, marking Dr. Robert Koch’s discovery of the TB-causing bacteria in 1882.
- The theme for World TB Day 2024 is Yes! We can end TB.
Tuberculosis (TB)
- Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis.
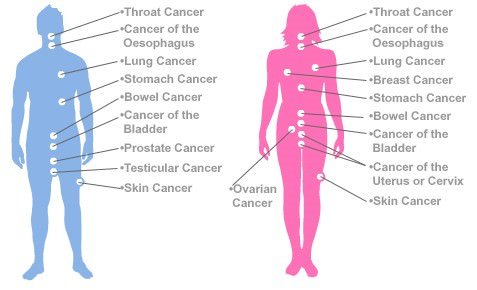
- TB commonly affects the lungs (pulmonary TB) but can also affect other parts (extrapulmonary TB).

- Pulmonary tuberculosis is a chronic consumptive disease that can be present as acute pneumonia.
- Pneumonia is an inflammatory lung condition affecting the microscopic air sacs known as alveoli.

- Transmission: It spreads from person to person through the air when people infected with TB cough, sneeze or otherwise transmit respiratory fluids through the air. However, people with latent TB (when the infections do not show any symptoms) do not spread the disease.
- The most common risk factor associated with TB is HIV and other conditions that impair the immune system.
Tuberculosis Symptomatic Diagnosis
- Most infections do not have symptoms, known as latent tuberculosis.
- About 10% of latent infections eventually progress to active disease that kills about half of those infected if left untreated.
Common symptoms include:
- Chronic cough with blood-tinged sputum
- Loss of weight
- Loss of appetite
- Fever and night sweats
- Fatigue are common symptoms of tuberculosis, etc.

TB Treatment
- The standard 6-month course treatment consists of 2 phases:
- 1st phase lasts 2 months and is called the Intensive phase.
- 2nd phase lasts for 4 months and is called the Continuous phase.
- For new TB cases, the treatment in the intensive phase (IP) consists of four drugs:
- Isoniazid (INH)
- Rifampicin
- Pyrazinamide
- Ethambutol
- For previously treated cases of TB, the intensive phase is 12 weeks, where an injection of streptomycin is given for eight weeks along with four drugs.
- A strictly followed 6-month drug regimen cures most people with TB.
Multidrug-Resistant TB (MDR-TB)
- CBNAAT (Cartridges Based Nucleic Acid Amplification Test) is used for early diagnosis of MDR-TB.
- In MDR-TB, the bacteria develop resistance to antimicrobial drugs used to cure the disease.
- MDR-TB does not respond to at least isoniazid and rifampicin, the 2 most powerful anti-TB drugs.
- Treatment options for MDR-TB are limited and expensive.
- In some cases, even more severe drug-resistant TB may develop.
Causes
- MDR-TB is caused due to mismanagement of treatment and person-to-person transmission.
- Mismanagement of TB treatment involves inappropriate or incorrect use of antimicrobial drugs or ineffective formulations of drugs and premature treatment interruption.
Extensively Drug-Resistant TB (XDR-TB)
- XDR-TB is a form of multidrug-resistant TB with additional resistance to more anti-TB drugs.
- People who are resistant to isoniazid and rifampicin, plus any fluoroquinolone and at least one of three injectable second-line drugs (amikacin, kanamycin, capreomycin) are said to have XDR-TB.
Treatment for Drug-Resistant TB
- The treatment success in MDR-TB is about 54%, while it is just 30% in the case of XDR-TB patients.
- A combination of eight drugs for over a year is needed for XDR-TB treatment.
- Treatment success in XDR-TB patients depends on the extent of the drug resistance, the severity of the disease, whether the patient’s immune system is weakened, and treatment adherence.
- Drugs used for treating MDR-TB and XDR-TB can cause serious adverse effects such as deafness.
The Goal to End TB by 2025
- Revised National TB Control Programme was renamed the National TB Elimination Programme.
- The name change aligns with the larger goal of eliminating the disease by 2025, five years ahead of the SDG 3.3 target.
World Health Organisation’s (WHO’s) Global TB Report 2023
- Severity: TB remained the world’s 2nd leading cause of death from a single infectious agent in 2022, after COVID-19. India reported a case fatality ratio of 12%.
- High-burden countries: 30 countries with a high TB burden make up 87% of global incident cases.
- Top 8 countries contribute 2/3rd of total cases: India, Indonesia, China, Philippines, Pakistan, Nigeria, Bangladesh, and the DR of the Congo.
- High reduction: 13 high-burden countries have registered major reductions in TB cases. These include India, Indonesia, and the Philippines.
- TB diagnosis and treatment: Though wide gaps persist, there was a major global recovery in the number of people diagnosed with TB and treated in 2022 after 2 years of COVID-related disruptions.
- High mortality without treatment: Without treatment, the death rate from TB is high (about 50%).
- Though with the WHO-recommended treatment, around 85% of TB patients can be cured.
Issues with TB Prevention and Treatment in India
Inadequate access to quality diagnosis
- WHO recommends molecular diagnostics as the initial test due to high accuracy, drug resistance detection, cost-effectiveness, and minimised treatment delays.
- But, last year in India, only 23% of suspected TB patients underwent these recommended tests.
- The remaining 77% underwent microscopy, a century-old tool that cannot detect drug resistance and detects only half of all people.
Emergence of drug-resistant TB
- Multidrug-resistant TB (MDR-TB) is caused by TB bacteria that are resistant to the two most powerful first-line anti-TB drugs, isoniazid and rifampicin.
- Extensively Drug-Resistant TB (XDR-TB) is a rare form of MDR-TB caused by TB bacteria that are resistant to several of the most effective anti-TB drugs.
- MDR-TB is caused due to mismanagement of treatment and person-to-person transmission.
- India recorded 1.1 lakh MDR-TB cases in 2022.
Non-adherence to treatment
- The treatment for TB is long and complex and even longer for MDR-TB.
- This discourages the patients from adhering to the complete treatment.
- The stigma associated with TB discourages patients from seeking care and completing treatment.
Shortage of drugs
- There have been reports of a shortage of TB treatment drugs in different states.
- After the rollout of a shorter TB Preventive Treatment (TPT) called the 3HP, states are yet to receive the 3HP combination drug from the Central TB Division.
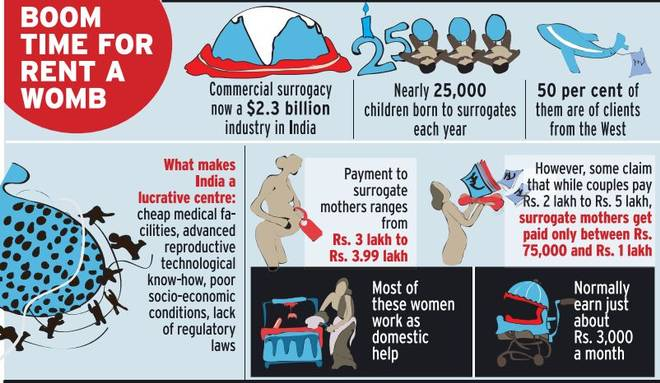
Social determinants of TB
- Poverty, malnutrition, and overcrowding increase susceptibility to TB infection.
- Marginalised communities, like tribals and migrants, are disproportionately affected by TB.
Suggestions to Improve Diagnosis
- To tackle TB, we need to improve diagnosis methods. This involves using existing systems better and adopting new technologies for quicker and more accessible diagnosis.
Need to utilise X-ray imaging during the screening procedures
- For example, India conducts active case-finding efforts nationwide. However, recent studies suggest that symptom-based screening alone may miss many TB cases, as some infected individuals show no symptoms but can still spread the disease.
- So, there is a need to utilise X-ray imaging that can quickly and efficiently find TB patients.
- X-ray imaging has improved significantly, with portable devices and AI-driven software that can quickly detect possible TB cases.
- New technologies like the urine LAM test offer rapid screening for both lung and extra-lung TB cases, aiding in effective population screening.
Need to use Molecular tests to confirm TB bacteria presence
- Molecular tests are faster and more precise than the traditional sputum microscopy test.
- India has increased its molecular diagnostic capacity, but these tests are costly and not easily accessible.
- The NAAT (nucleic acid amplification test) machines in India have gone up from 651 in 2017 to more than 5,000 in 2022.
- Challenges: Molecular testing is reliant on sputum collection and testing. Collecting sputum samples poses challenges, especially for children, and transporting samples in remote areas is difficult.
Need to explore other collection techniques
- During the COVID-19 pandemic, simpler testing methods like nasal swabs and saliva samples increased testing coverage.
- We should consider using tongue swabs for TB sample collection, which is simple and cost-effective.
- PCR machines, proven useful during COVID-19, can also be utilised for TB diagnosis across the country.
10-Point Agenda to Control TB in India
- Early Detection and Screening: Early detection is crucial for TB, as symptoms are often ignored. Screening of family and contacts of infected individuals is vital, requiring accessible lab facilities and efficient follow-up systems.
- Precise Treatment Categorization: This is essential due to the increasing number of drug-resistant TB cases. Knowing resistance status at diagnosis helps assign appropriate treatment.
- Treatment Adherence and Monitoring: TB treatment requires a long duration, so non-compliance can occur due to various reasons, like health improvement or relocation. It is important to use technology to monitor compliance.
- Preventing TB-related deaths: whether from drug-resistant or non-pulmonary TB, is critical.
- Controlling Drug Resistance: This is crucial as it’s often caused by the misuse of antibiotics and non-compliance with treatment. Poor regulation of drug use and treatment non-compliance contribute to drug resistance.
- Assessing Extent of Drug-Resistant TB: This includes rifampicin-resistant TB (RR-TB) and multidrug-resistant TB (MDR-TB). This data helps plan the control program, allocate resources, and ensure trained staff are available.
- Ensuring Availability of Medicines: Procurement challenges for medications like bedaquiline and delamanid must be addressed. Treatment facilities for all drug-resistant TB cases requiring in-patient care should also be ensured.
- Integration into Health Systems: Strengthening referral networks between different levels of public and private health systems ensures no symptomatic cases are missed, patients take their medications, and contacts of TB cases are screened.
- Implementing a Dynamic Notification System: This will ease the burden on health system personnel. While Ni-kshay, a patient management system for TB, has evolved, improvements are required to capture real-time TB data across sectors, practitioners, and locations.
- Addressing Population Mobility: TB treatment should be portable within the country to ensure patients can resume their daily activities quickly after diagnosis and treatment initiation.
Other strategies for enhancing TB Control in India
- Focus on providing nutritional support. Research shows that improving nutrition reduces TB cases among household contacts of infected individuals.
- Addressing stigma and gender-related aspects of TB.
- More testing facilities, especially in rural areas.
- TB drugs should be free, affordable, and of good quality.
- Community-based care models need to be strengthened to address social, economic, and mental health needs.
- Frontline health workers should be empowered to provide comprehensive care closer to where patients live.
- India can improve treatment outcomes by supporting frontline workers, improving supply chains, decentralising services, and empowering local communities.
- Need for a multi-sectoral approach addressing poverty, nutrition, housing, and air quality.
- Using technology like AI and digital health can improve TB diagnosis, treatment adherence, and surveillance in India.
- Developing better vaccines is key to eliminating TB in the long run.
Initiatives Taken by India against TB
National TB Elimination Programme (NTEP)
- 1962: GoI launched National TB Programme (NTP) with BCG vaccination at the district level.
- 1993: WHO declared TB a global emergency and devised the directly observed treatment (DOTS).
- 1993: GOI revitalised NTP as the Revised National TB Control Programme (RNTCP).
- 1997: DOTS was launched as the RNTCP strategy. By 2006 the entire country was covered.
- In its second phase (2006–11), RNTCP improved the quality and reach of services.
- Despite the measures, undiagnosed and mistreated cases continued to drive the TB epidemic.
- A large number of MDR-TB cases were reported every year.
- To address this, National Strategic Plan for Tuberculosis Control 2012-2017 was documented with the goal of ‘universal access to quality TB diagnosis and treatment’.
- Significant interventions were taken during NSP 2012-2017 regarding mandatory notification of all TB cases, integration of the programme with the National Health Mission, etc.
- To eliminate TB in India by 2025, National Strategic Plan for Tuberculosis Elimination 2017-2025 involving all the stakeholders was formulated by RNTCP.
- On 01-01-2020, RNTCP was renamed National TB Elimination Programme (NTEP).
National strategic plan for tuberculosis elimination (NSP) 2017-2025 (NSP)
- TB elimination has been integrated into the four strategic pillars of “Detect – Treat – Prevent – Build”.
Detect
- Early diagnosis and treatment of TB are essential in TB elimination.
- The objective of NSP was to find all drug-sensitive TB cases and drug-resistant TB cases.
- To facilitate TB notification, RNTCP has developed a TB surveillance system called “NIKSHAY” (https://nikshay.gov.in) for government and private healthcare facilities.
- For TB diagnosis, more than 14,000 designated microscopy centres are spread across the country.
- Cartridge Based Nucleic Acid Amplification Tests (CBNAAT) / Line Probe Assay (LPA) has been established at district levels for decentralised molecular testing for drug-resistant TB.
- From 2020, GOI will use the Truenat test for early-stage diagnosis.
Treat
- Screening all patients for rifampicin resistance (and additional drugs wherever indicated) is done.
- For drug-sensitive TB, daily fixed-dose combinations of first-line anti-tuberculosis drugs are given.
Prevent
- Isoniazid Preventive Therapy (IPT) is given to children in close contact with a TB patient.
- BCG vaccination is provided at birth or as early as possible till one year of age. BCG vaccine protects against meningitis and disseminated TB in children.
Build
- Health system strengthening for TB control under the NSP 2017-2025 is recommended in the form of building and strengthening enabling policies, empowering institutions, and human resources.
Pradhan Mantri TB Mukt Bharat Abhiyan
- It is an initiative launched by the Ministry of Health and Family Welfare (MoHFW).
- It aims to eliminate TB from India by 2025 (5 years earlier than the global target of 2030).
- Objectives
- Provide additional patient support to improve treatment outcomes of TB patients
- Leverage Corporate Social Responsibility (CSR) activities
- The Ni-kshay Mitra shall provide additional support to all the on-treatment TB patients who have given consent for support.
- Ni-kshay Mitra can be a cooperative, corporate, elected Representative, individual, institution, NGO, or political party.
- The type of additional assistance that may be provided by the Ni-kshay Mitra include:
- Nutritional support
- Additional investigations for the diagnosed TB patients
- Vocational support
- Additional nutritional supplements
- The minimum commitment period for additional support to the TB patient is one year.
Ni-kshay Poshan Yojana
- Ni-kshay Poshan Yojana was launched by MoHFW in 2018 as part of the National TB Elimination Programme (NTEP).
- The scheme is centrally sponsored under the National Health Mission (NHM).
- A financial incentive of Rs.500/month is provided to each notified TB patient for the duration the patient is on anti-TB treatment.
- The incentives can be distributed in cash only via Direct Benefit Transfer (preferably through Aadhaar-enabled bank accounts) or in-kind.
Ni-kshay Portal
- It is the web-enabled patient management system for TB control under the National Tuberculosis Elimination Programme (NTEP).
- It is developed and maintained by the Central TB Division (CTD), MoHFW, in collaboration with the National Informatics Centre (NIC) and the WHO Country Office for India.
Bacillus Calmette-Guérin (BCG) Revaccination
- The Bacillus Calmette-Guérin (BCG) Vaccine is typically given to infants to protect them from TB.
- However, the effectiveness of the vaccine can wane over time.
- India now wants to implement BCG revaccination at scale; 23 states have already consented.
- There is currently no consensus on whether or not BCG revaccination is effective.
- WHO does not currently recommend BCG revaccination for any person.

![PMF IAS Environment for UPSC 2022-23 [paperback] PMF IAS [Nov 30, 2021]…](https://pmfias.b-cdn.net/wp-content/uploads/2024/04/pmfiasenvironmentforupsc2022-23paperbackpmfiasnov302021.jpg)