Antimicrobial Resistance, Causative Factors, Measures Taken
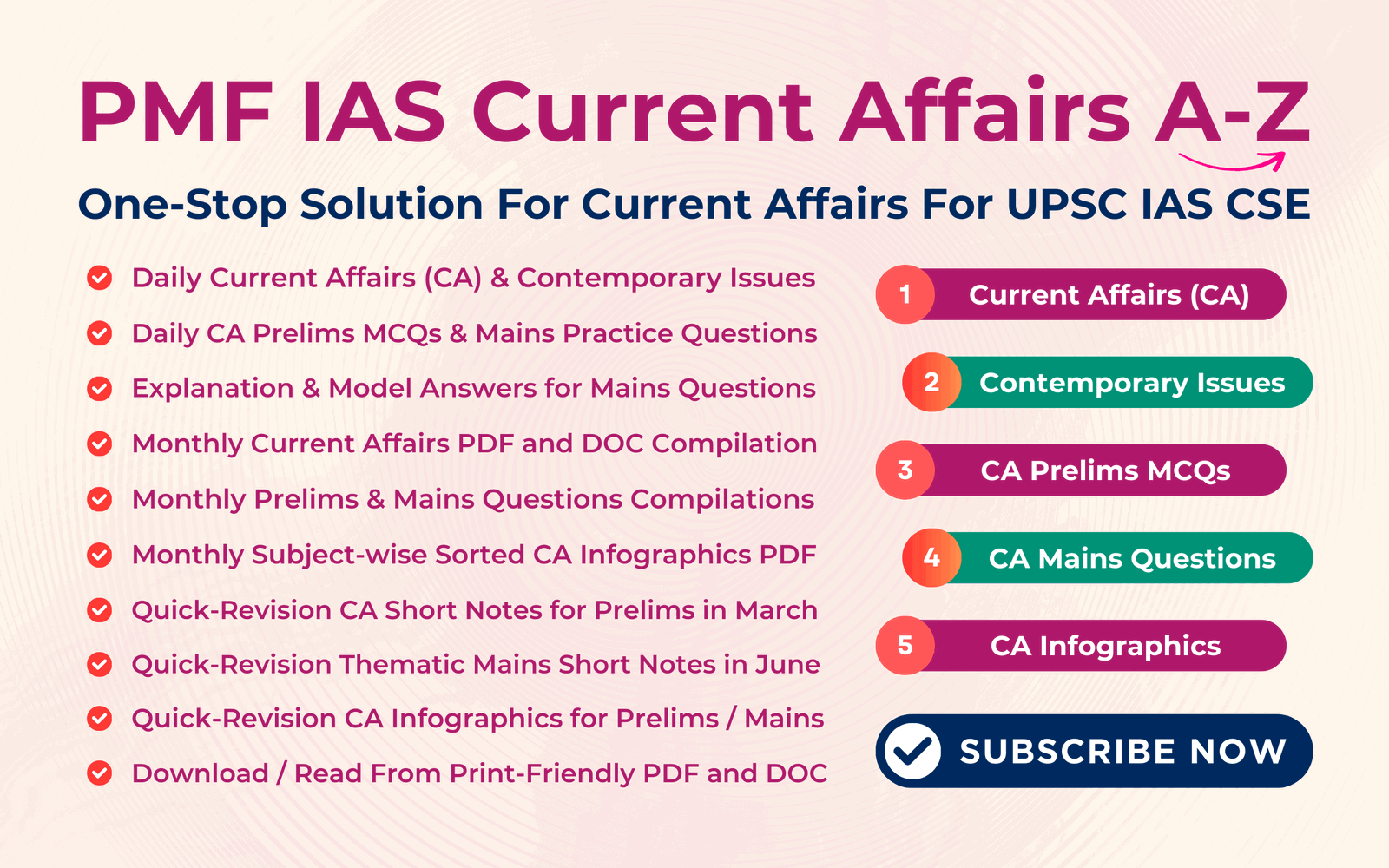
Subscribe to Never Miss an Important Update! Assured Discounts on New Products!
Must Join PMF IAS Telegram Channel & PMF IAS History Telegram Channel
What is Antimicrobial Resistance (AMR)?
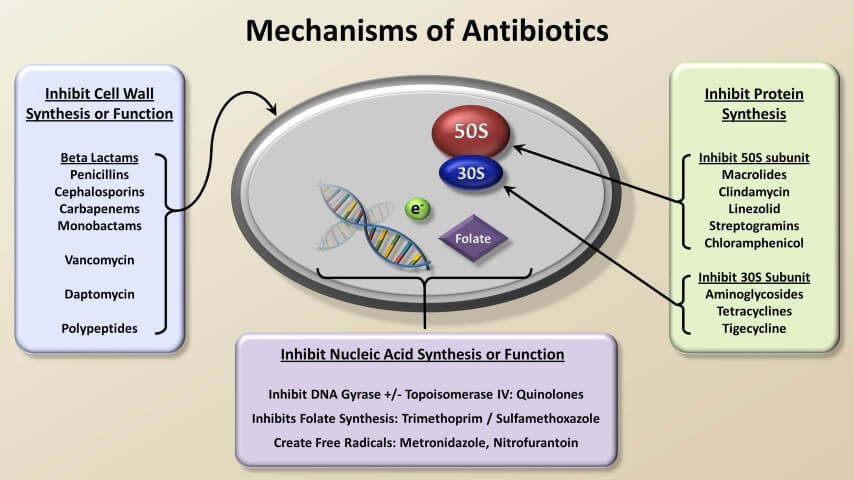
- Antimicrobials include antibiotics, antiviral, antifungal & anti-parasitic medication.
- The WHO defines antimicrobial resistance (antibiotic, antiviral, antimalarial resistance) as a microorganism’s resistance to an antimicrobial drug that was once able to treat an infection by that microorganism.
- E.g., In Multi-Drug Resistant TB (MDR-TB), the TB bacteria are resistant to two of the most important TB drugs, isoniazid (INH) and rifampicin (RMP).
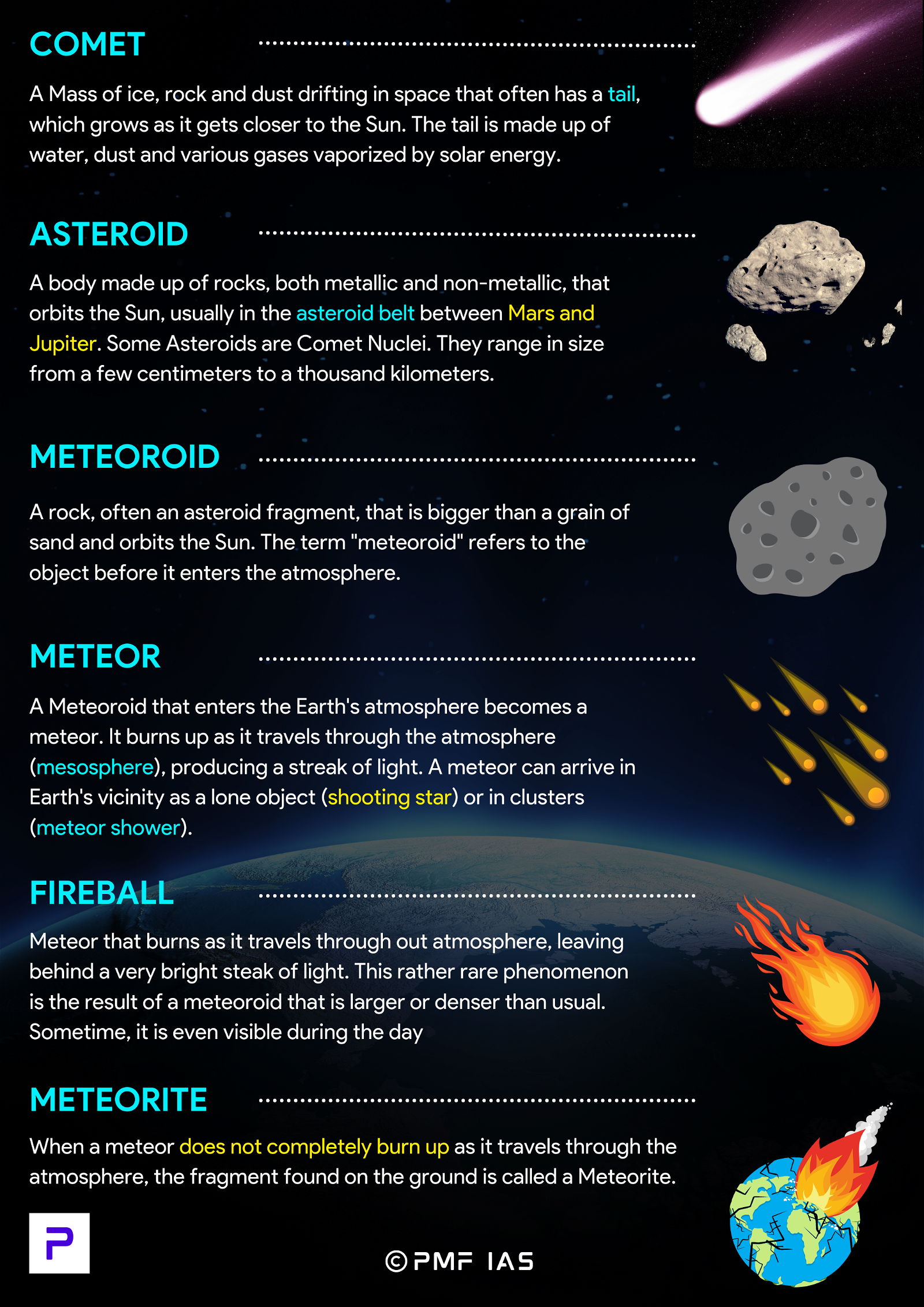
- Artemisinin-based combination therapies (ACTs) are the recommended first-line treatment for uncomplicated P. falciparum malaria & are used by most malaria-endemic countries.
- Partial resistance to Artemisinin has been confirmed in South-East Asia.
Causative Factors for Antimicrobial Resistance
- Antimicrobial resistance occurs when bacteria, viruses, fungi & parasites change over time & no longer respond to medicines.
- They become Superbugs and become resistant to the drugs that should usually destroy them.
- Micro-organisms can develop resistance mainly in two ways:
- Intrinsic resistance: Ability of an organism to resist a class of antimicrobial agents.
- Acquired resistance: Micro-organisms acquiring the gene coding (genetic mutation) for resistance.
- Intrinsic Antimicrobial resistance (AMR) occurs naturally over time, usually through genetic changes.
- Acquired resistance is more common than intrinsic resistance.
Causes Behind Acquired Antimicrobial Resistance
- Overuse, misuse, and improper use (e.g., taking antibiotics to treat viral diseases!) of antimicrobials.
- Greater access to over-the-counter antibiotic drugs in developing countries.
- Using broad-spectrum antibiotics over narrow-spectrum antibiotics (targeting specific microbes only).
- Dumping of inadequately treated effluents from the pharmaceutical industry.
- Antibiotic use in livestock feed at low doses for growth promotion is industrialized countries.
- Poor sanitation and hygiene that forces the extended use of antimicrobials.
World’s rivers loaded with antibiotics waste
- The concentrations of major antibiotics like Ciprofloxacin (treatment for intestinal and urinary tract infections) and metronidazole in water bodies were several times above the limit in many parts of the world.
Colistin in the food industry
- Colistin is a valuable, last-resort antibiotic that saves lives in critical care units.
- Colistin is as growth supplement (growth factor) in poultry & animals.
- In recent years, may patients have exhibited resistance to the drug.
- If colistin-resistant bacteria are found in the blood, there is 80% chance of death.

Why are Antibiotics effective against Bacterial Infections but not Viral Infections?
Why is it harder to make antivirals compared to antibiotics?
|
Concerns Raised Due to Antimicrobial Resistance
- As a result of drug resistance, it has become increasingly difficult or impossible to treat some diseases.
- Treating resistant microbes require alternative or higher doses of medication (expensive + toxic).
- In 2016, upto 4,90,000 people developed multi-drug-resistant TB globally.
- Drug resistance is starting to complicate the fight against HIV and malaria.
- Organ transplantation, chemotherapy & surgeries would be compromised without effective antimicrobials.
- Medical procedures, such as surgery have become riskier.
- Antimicrobial resistance increases the cost of health care with lengthier stays in hospitals, additional tests & use of more expensive drugs.
- It can ultimately lead to Antibiotic Apocalypse – A future without antibiotics, with bacteria becoming completely resistant to treatment & when common infections & minor injuries could once again kill.
Measures Required
- Global collective action through international treaties on antimicrobial resistance.
- Preventing over the counter sale of antibiotics.
- Swatch Baharat, awareness, etc.
Steps taken Globally to fight Antimicrobial Resistance
Global Action Plan on Antimicrobial Resistance (GAP)
- Globally, countries committed to the framework set out in the Global Action Plan (GAP) 2015 on AMR during the 2015 World Health Assembly.
- t mandated nations to develop & implement national action plans to tackle microbial resistance.
Tripartite Joint Secretariat on Antimicrobial Resistance
- A tripartite joint secretariat (FAO, World Organisation for Animal Health (OIE) & WHO) is established in 2016.
- It aims to drive multi-stakeholder engagement in AMR.
World Antimicrobial Awareness Week (WAAW)
- Held annually since 2015.
- It is a global campaign that aims to raise awareness of antimicrobial resistance worldwide.
The Global Antimicrobial Resistance & Use Surveillance System (GLASS)
- It was launched by WHO in 2015 to continue fill knowledge gaps & to inform strategies at all levels.
- It is conceived to progressively incorporate data from surveillance of AMR in humans, medicines, food chain & in the environment.
Global Research & Development priority setting for AMR
- In 2017, to guide research & development into new antimicrobials, diagnostics & vaccines, WHO developed the WHO priority pathogens list.
- It will be updated in 2022.
Global Antibiotic Research & Development Partnership (GARDP)
- A joint initiative of WHO & the Drugs for Neglected Diseases Initiative (DNDi).
- The partnership aims to develop & deliver 5 new treatments that target drug-resistant bacteria identified by WHO as posing the greatest threat by 2025.
Steps taken by India to Fight Antimicrobial Resistance
- India formed National Action Plan to combat Antimicrobial Resistance.
- The National Health Policy 2017 highlights the problem of antimicrobial resistance & calls for effective action to address it.
- Since 2014 a separate Schedule H-1 has been incorporated in Drug & Cosmetic rules to regulate the sale of antimicrobials in the country.
- Health Ministry initiated Red Line Campaign:
- It urged people not to use the medicines marked with a red vertical line without prescription.
- The Food Safety & Standards Authority of India (FSSAI) banned the use of antibiotics & several pharmacologically active substances in fisheries.
2019: Colistin banned in animal food industry
- The Ministry of Health and Family Welfare has prohibited the manufacture, sale and distribution of colistin and its formulations for food-producing animals, poultry, aqua farming and animal feed supplements.
- The move is a “massive victory” for the movement against anti-microbial resistance.
National Action Plan – India
- National Action Plan to combat Antimicrobial Resistance is on the lines with World Health Organization’s Global Action Plan (GAP) for AMR.
- The plan highlights the need for tackling AMR across multiple sectors such as human health, animal husbandry, agriculture & environment in consideration of the “One-Health” approach.
Priority Areas
Education & Training
- Revision of curriculum for professionals in animal, agriculture & environment sector with focus on AMR.
Surveillance
- Conducting national-level surveillance of antibiotic residues in food from animals & in environment.
Infection Prevention & Control
- Restricting antibiotics in animal feed, & regulating their import, direct distribution & online marketing.
- Eliminating use of critically important antimicrobials for humans in food animals.
- Ensuring prescription sale of antibiotics & appropriate labeling of food from animals produced with or without routine use of antibiotics.
Environment
- Strengthening of necessary laws & regulations, environment risk assessment; extended producer responsibility for expired/unused antibiotics.
Mains Practice: “Anti-Microbial Resistance is a complex global problem & requires multi-faceted approach”. Discuss (250 Words)
Paid users of Science & Technology Notes can download the above content from Sci & Tech May 2021 Current Affairs